Left Breast & SCF Treatment: Radixact® System and VitalHold™ in Deep Inspiration Breath Hold (DIBH)
Bilateral Breast Irradiation with Simultaneous Integrated Boost Technique
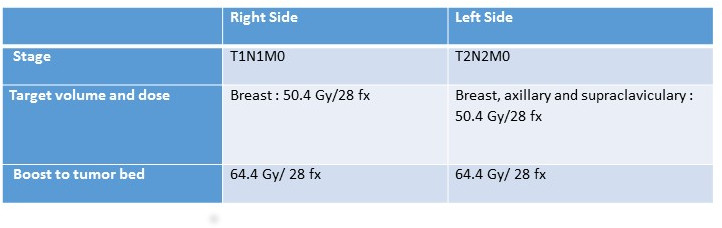
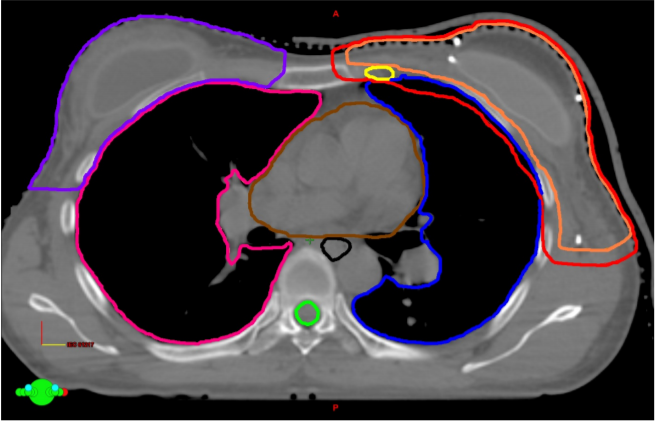
A 46-year-old female patient attended to at the hospital for a painless mass at upper quadrant of left breast. A detailed physical examination also revealed another suspected mass at right breast. The ultra sonographic evaluation demonstrated two different suspected tumors at both breasts. There were no distant metastasis observed in positron emission tomography. Biopsy taken from right breast was diagnosed as invasive lobular carcinoma. In ‘tumor board’, patient was discussed in detail, and breast-conserving surgery and sentinel lymph node dissection was planned. Postsurgical pathological evaluation reported invasive lobular carcinoma at right and left breasts, with T1N1M0 and T2N2M0 stages, respectively.
Postoperative treatment plan included 8 cycles of chemotherapy and local radiotherapy (RT), thereafter. The tumor stages and RT plans are summarized in Table 1.
Right Breast Invasive Ductal Carcinoma treated with Stereotactic Partial Breast Irradiation (S-PBI)
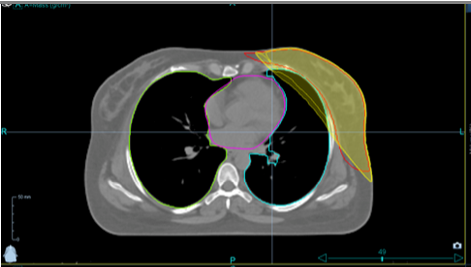
A 43-year-old Caucasian woman presented with a density in the right breast at 6 o’clock on screening mammogram in 2012. Follow up sonography revealed a 1.4 cm hypoechoic mass. Sono-guided core biopsy led to diagnosis of infiltrating ductal carcinoma that was grade 2, cT1cN0M0, and stage 1 with associated atypical ductal hyperplasia. Tumor was ER 100%, PR 100%, HER-2 negative, and had Ki-67 of 17%. Genetic testing was negative for BRCA1 and BRCA2 mutation. Patient reported no breast mass, skin change, or nipple discharge.
A partial mastectomy was performed and four axillary sentinel lymph nodes sent for sampling. Four gold fiducials were also placed at the time of surgery around the lumpectomy cavity. The first was placed inferiorly and very close to the chest wall since the cancer was located near the inframammary fold. Superior, medial and lateral fiducials were placed and staggered in such a way so that none of them would occur on the same axial or transverse slice through the breast. Four titanium clips were also placed to mark the boundaries of the excision cavity at the time of surgery.
Pathology results were consistent with pT1cN0M0 grade 2 stage 1 invasive ductal carcinoma and associated intermediate nuclear grade ductal carcinoma in situ. There was no lymphovascular invasion and margins were widely negative. Tumor was ER 32%, PR 86%, HER-2 negative, and Ki-67 of 7%.
Radiation treatment was postponed to 9 weeks due to delayed wound healing of the lumpectomy scar. A superficial 2 mm opening with drainage was infected with staph aereus for which the patient was put on antibiotics. Signs of skin infection cleared, and the skin wound was fully healed by the time she started stereotactic body radiation therapy with Cyberknife on our phase I institutional 5 fraction dose escalation trial.
CyberKnife for accelerated partial breast irradiation

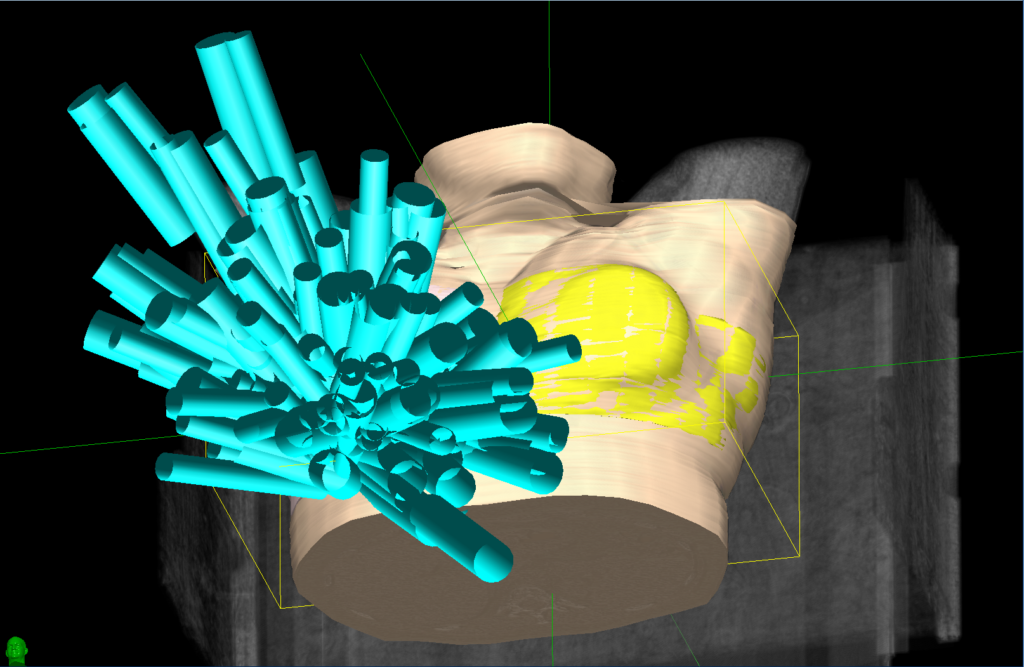
This 60-year-old woman presented with right breast mass in lower central quadrant. Biopsy under ultrasonography demonstrated invasive ductal carcinoma with ER positive (100%), PR positive (80%). Further work up revealed no metastatic axillary lymph node. Patient was referred for partial mastectomy with sentinel lymph node biopsy. Final pathology report for surgical specimen demonstrated 1.3 cm sized invasive ductal carcinoma with histologic grade 2 without extensive intraductal component, lymphovascular space invasion and metastatic lymph node (of 2 sentinel nodes). The maximum diameter of invasive and in situ carcinoma was 1.5 cm. In addition, negative resection margin was achieved. Finally, she was categorized as “suitable” and “low-risk” group under the ASTRO and GEC-ESTRO guideline, respectively then we decided to perform accelerated partial breast irradiation.
To reduce set-up uncertainty, contralateral/ipsilateral breast radiation dose, and treatment time, we chose to use the CyberKnife system with fiducial tracking mode and MLC for accelerated partial breast irradiation.
Helical TomoTherapy for Postmastectomy Radiotherapy after Immediate Left Breast Reconstruction: A Case Study